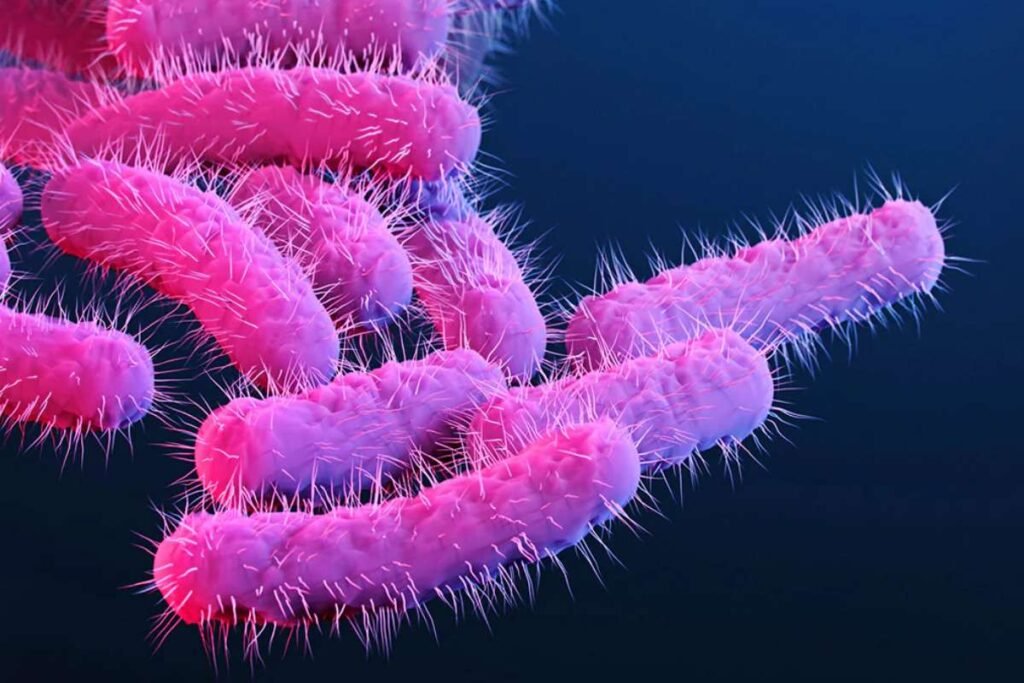
Rising Cases of Shigella Linked to Lack of Sanitation Facilities
Multnomah County is witnessing a concerning rise in cases of Shigella infections, a bacterial disease known for causing severe diarrhea, fever, and vomiting. The county reported 158 cases in 2024, nearly doubling from the previous year, with 40 cases recorded in January alone. Health experts believe the actual number of infections may be higher, as many affected individuals do not seek medical care.
The surge in cases has been largely attributed to the county’s worsening homelessness crisis. People experiencing unsheltered homelessness often lack access to proper sanitation, increasing their risk of contracting and spreading the highly contagious disease. Dr. Amanda Risser, senior medical director at Central City Concern, emphasized the need for handwashing facilities, stating, “Any situation where you are unable to wash your hands regularly puts you at risk for shigella.”
Dr. John Townes, medical director for infection prevention at Oregon Health & Science University, stressed that improving public hygiene infrastructure is a crucial step in controlling the outbreak. “If you want to stop an outbreak of shigella, you give people toilets, soap, and water,” he said. However, with only about 116 publicly maintained restrooms in Portland and an estimated 6,000 people living outside, access to hygiene facilities remains insufficient.
Public Health Challenges and Impact on Vulnerable Communities
Health professionals and sanitation workers in Portland have observed a stark increase in public defecation, further escalating health risks. Risser noted that she encounters human waste on city streets daily, an issue that she believes stems from the lack of public restrooms rather than drug use. Adam Solano, dispatch manager for Ground Score, which cleans Portland’s streets, reported receiving multiple daily calls about human waste removal, requiring the city’s biohazard team to intervene.
Shigella spreads easily, especially in group settings, where shared facilities increase transmission risks. One recent outbreak occurred at a wedding, where a food preparer who had not washed their hands infected multiple guests. Another case involved J.W. Mosher, a sanitation worker who contracted the disease while cleaning toilets at a residential facility in Southeast Portland. He described suffering from “uncontrollable diarrhea for two weeks” before seeking medical attention.
Multnomah County data reveals that since 2017, 44% of shigellosis cases not linked to foreign travel occurred among people without stable housing. More recently, that figure has risen to 56%. The county also noted that drug users and men who have sex with men are overrepresented in confirmed cases. Health officials continue to monitor the situation closely, offering priority medical appointments to affected individuals in high-risk settings.
Efforts to Contain the Outbreak of Cases of Shigella and Future Preventive Measures
Efforts to curb the outbreak have faced logistical and social barriers. A past attempt to address the sanitation crisis by deploying portable toilets in high-risk areas was met with public resistance. Vandalism and theft rendered many of the units unusable, and some housed residents actively opposed their installation. City officials now hesitate to reintroduce similar measures, citing prior backlash and maintenance challenges.
Meanwhile, calls to reopen public restrooms during winter have been met with financial and infrastructural hurdles. Portland Parks Bureau spokesperson Mark Ross explained that many park restrooms are not winterized and could suffer damage from freezing temperatures. Retrofitting them for year-round use would require significant funding, which the city currently lacks.
Despite these challenges, the county has launched a communicable disease supportive housing program to provide temporary shelter for those infected with contagious illnesses like shigella. Since its inception, 24 people—20 of whom had shigellosis—have received housing support through the initiative. The program aims to help 50 people by June, reducing the spread of infectious diseases in vulnerable communities.
While most Cases of Shigella infections resolve on their own, severe cases require medical intervention. Health officials urge individuals to practice proper hygiene, drink plenty of fluids, and seek medical care if symptoms persist for more than two days. Experts warn that antibiotic resistance among certain shigella strains complicates treatment, making prevention through sanitation and hygiene the best defense against further outbreaks.