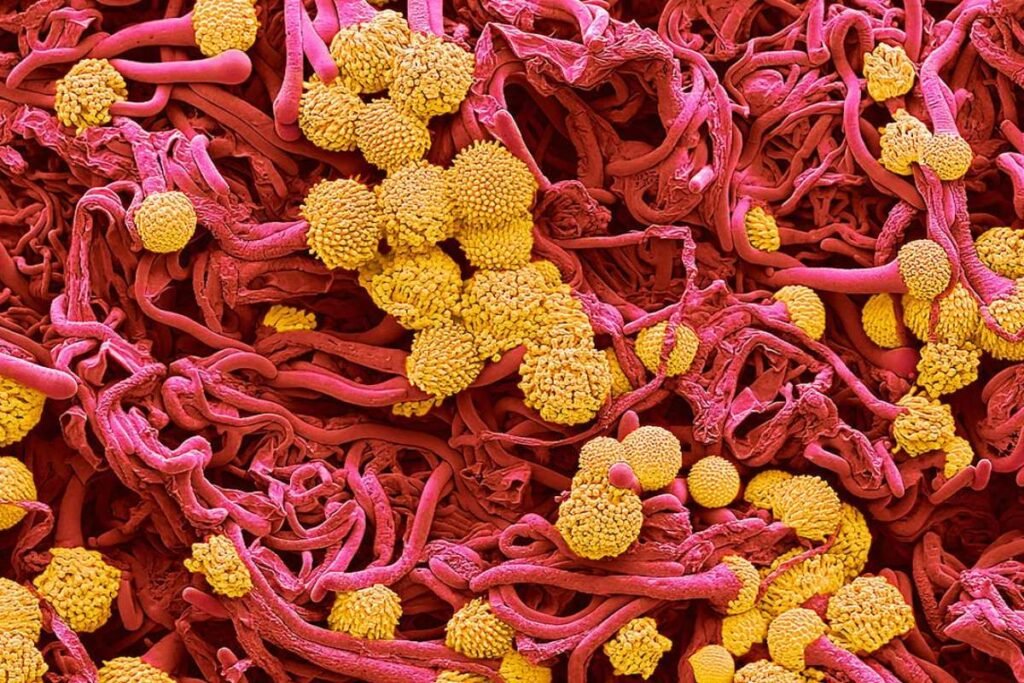
A deadly airborne Lethal Fungus , Aspergillus fumigatus, is rapidly spreading across the United States, alarming health experts and putting hundreds of thousands of lives at risk. Known for its capacity to “eat” human tissue from within, the lethal fungus causes a severe lung infection called aspergillosis, which can lead to organ failure and death in vulnerable individuals. The most at-risk groups include those with weakened immune systems, such as cancer, asthma, or HIV patients, who can unknowingly inhale the microscopic spores.
States with warm, humid conditions like Florida, Texas, Georgia, Louisiana, and California are seeing the highest levels of fungal presence, especially in areas with extensive farming. Large urban centers like New York, Houston, and Los Angeles are also facing increased exposure due to their dense populations and aging infrastructure. Despite the growing threat, aspergillosis remains a non-reportable disease in the U.S., meaning that cases and fatalities often go undocumented. This underreporting hampers early detection and public awareness.
Doctors are urging high-risk individuals to avoid activities that may expose them to spores, such as gardening or contact with moldy environments. Precautions like using masks in dusty areas and maintaining clean air filtration in homes and hospitals are also being encouraged. In response, U.S. hospitals have intensified their mold monitoring and implemented stricter antifungal protocols.
Climate Change and Drug Resistance Intensify the Threat
The rapid spread of Aspergillus fumigatus is being exacerbated by rising global temperatures, which enable the lethal fungus to thrive both outdoors and inside the human body. The organism can withstand extreme conditions, including temperatures exceeding 120°F, particularly in compost and soil. Scientists warn that with continued fossil fuel emissions, the lethal fungus’s range could expand by over 75% by the year 2100, especially affecting the southern United States.
Norman van Rhijn, a co-author of a major University of Manchester study, highlighted the urgency of the issue, warning that “in 50 years, where things grow and what you get infected by is going to be completely different.” Currently, about 400,000 cases of chronic pulmonary aspergillosis are reported annually, but the invasive form, though less common, is far more fatal. It spreads from the lungs to vital organs and has particularly devastating outcomes among transplant recipients. One study showed that only 25% of stem cell transplant patients survived a year after infection.
Hospitalizations for invasive aspergillosis rose by about 3% annually from 2000 to 2013, with nearly 15,000 stays recorded by 2014, amounting to a financial burden of $1.2 billion. The World Health Organization now lists Aspergillus fumigatus as a “critical priority” threat due to its growing drug resistance and high mortality rate.
Calls for Urgent Action and Research Investment
The overuse of azole-based antifungal drugs, commonly employed in both human medicine and agriculture, is contributing significantly to rising drug resistance. Recent studies have found azole-resistant Aspergillus fumigatus strains in farm soils across at least seven U.S. states, with many strains no longer responding to standard treatments. Scientists believe the cross-contamination between environmental and clinical fungal strains is accelerating resistance, posing a serious challenge to current treatment strategies.
In light of these developments, health experts and global organizations are calling for immediate investment in safer and more effective antifungal medications. The WHO is urging pharmaceutical companies to prioritize fungal research, improve diagnostic capabilities, and expand clinical trials to include children. Dr. Vyas, an infectious disease expert at Columbia University, summarized the growing concern: “This isn’t science fiction. These infections are real, and we’re not ready.”
With the threat mounting from both nature and negligence, the U.S. faces a critical moment to address the fungal epidemic before it becomes an unmanageable public health crisis.