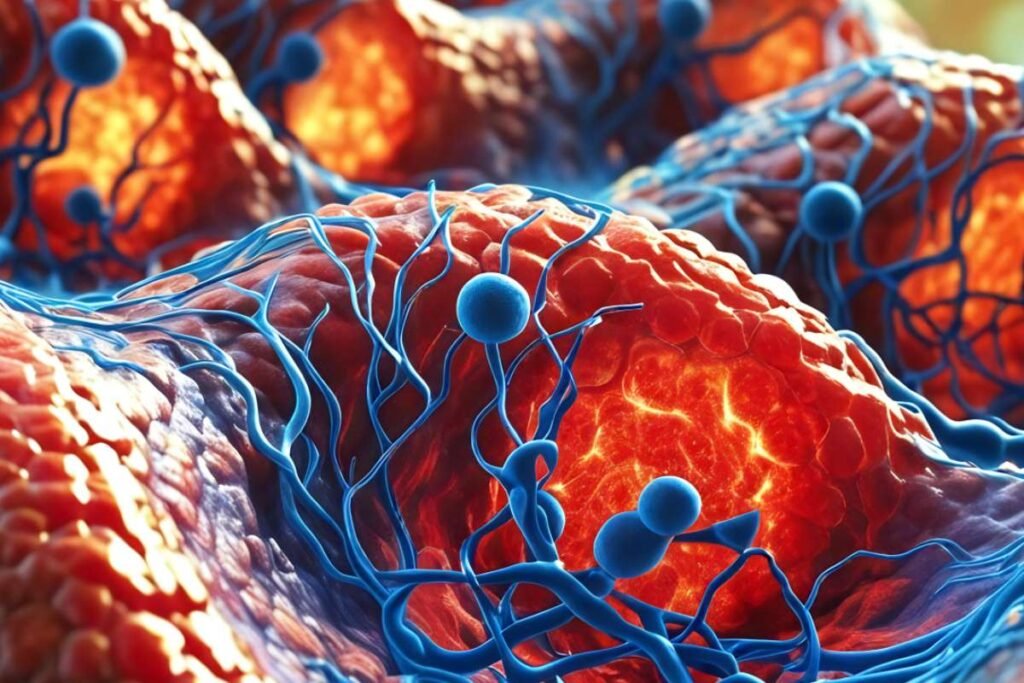
A 36-year-old Canadian nurse, Amanda Smith, has stunned the medical world by coming off insulin completely following a single experimental Stem Cell Therapy treatment. Diagnosed with Type 1 diabetes a decade ago, Smith had been managing the autoimmune condition with a demanding routine of insulin injections, diet monitoring, and blood sugar tracking. On February 14, 2023, her life took a dramatic turn when she received an injection of lab-grown, insulin-producing islet cells into her liver.
By August that year, Smith no longer required insulin. Nearly two years on, she remains insulin-free. Speaking to CTV News, an emotional Smith said, “I get emotional because I’m free from those handcuffs… I don’t have that looming over me every day.” Her story has offered hope to millions living with the burdens of Type 1 diabetes, a condition that typically begins in childhood and has no known cure.
A Landmark Moment in Type 1 Diabetes Treatment
Smith was among 12 participants in an experimental trial of the new stem cell-based treatment. Of those, 10 are now reportedly off insulin entirely. The success of this Stem Cell Therapy has been hailed as a major medical milestone. “The data is just so fascinating, so very, very powerful,” said Dr. Peter Senior, director of the Alberta Diabetes Institute, though he was not involved in the study. “They blew past the objectives.”
The goal of the trial was to prove better blood sugar control and reduced incidents of severe hypoglycemia. The outcomes surpassed expectations, with the majority of participants experiencing complete insulin independence. Experts believe the potential for a transformative shift in diabetes treatment is now within reach, marking a significant leap from the conventional insulin-based management that has remained unchanged for a century.
Challenges Ahead for Widespread Use
Despite the promising results, the treatment is not yet ready for mass adoption. One major hurdle is the body’s immune response. Whether derived from donors or created in labs, these islet cells are often seen as foreign by the immune system, necessitating the use of strong immunosuppressive drugs. These drugs carry their risks, including vulnerability to infections, organ damage, and even cancer.
Furthermore, before full regulatory approval from bodies like the FDA can be granted, extensive clinical trials are required. These trials are both expensive and time-consuming, with safety and long-term efficacy needing robust confirmation. Additionally, the therapy’s cost and complexity present further barriers to broad accessibility.
Nevertheless, medical experts are optimistic. “We’ve got potentially a limitless source of cells that could be used,” Dr. Senior noted. “This is a massive, huge step forward in terms of a cell therapy becoming a reality.” As the research advances, it may one day offer a lasting, transformative solution for millions living with Type 1 diabetes.