(Source-NPR)
A recent update from the U.S. Preventive Services Task Force has stirred conversations by recommending earlier and more frequent mammogram screenings for women. The updated guidelines suggest women aged 40 to 74, with an average risk of breast cancer, undergo screening every two years. This adjustment, replacing the previous recommendation for individual screening decisions in one’s 40s and commencement no later than age 50, has sparked inquiries among women seeking clarity on its implications for personal health.
Exploring the Motivation behind the Change:
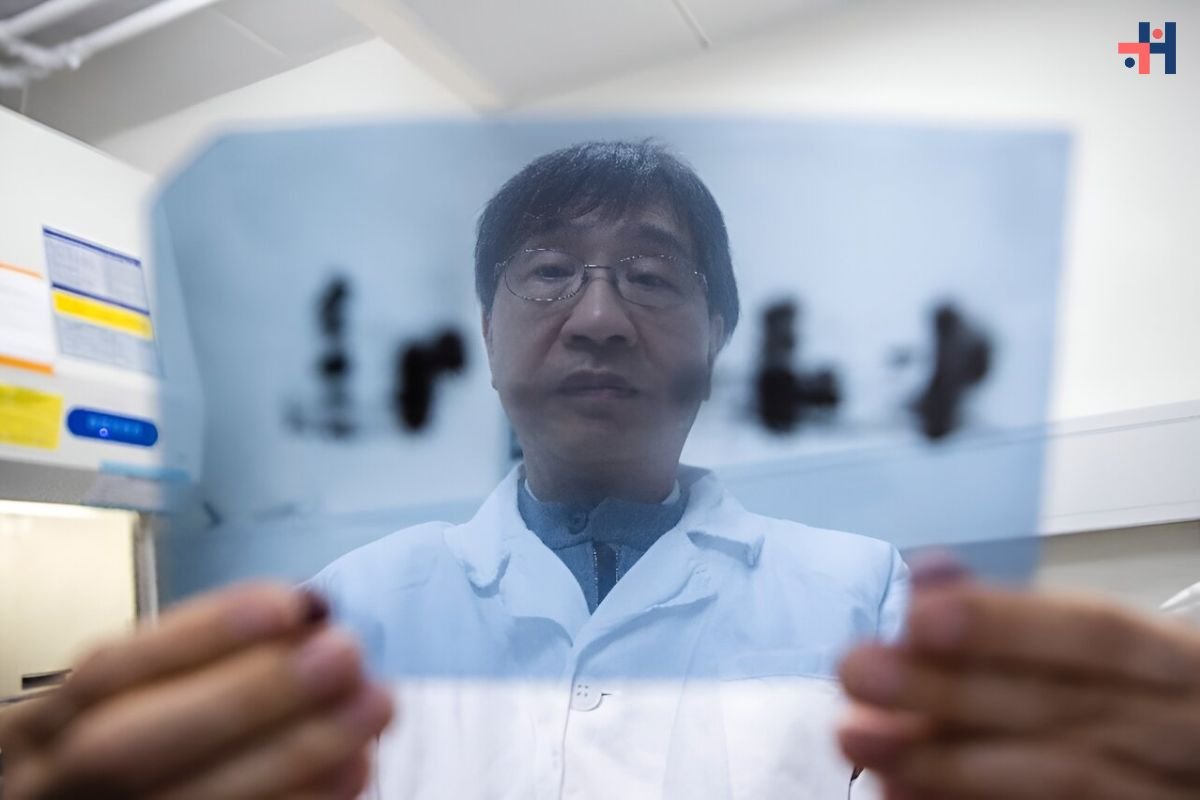
The rationale behind the modified guidelines stems from escalating cancer rates among younger demographics, particularly evident in the rising incidence of breast cancer among women in their 40s. According to John Wong, a professor of medicine at Tufts University School of Medicine and vice-chair of the task force, the numbers of newly diagnosed cases among this age group have been increasing by approximately 2 percent annually. Furthermore, the disparities in breast cancer diagnosis and mortality rates between Black and White women have underscored the urgency for targeted interventions.
Aim to Address Disparities and Save Lives:
The revised recommendations not only aim to curb the upward trend in breast cancer rates among younger women but also to bridge racial disparities in diagnosis and outcomes. By initiating screening at an earlier age, the task force anticipates potentially saving up to 20 percent of women from succumbing to breast cancer.
While the updated guidelines provide clear directives for screening in the 40 to 74 age bracket, they refrain from offering specific recommendations for women beyond the age of 74. The task force cites insufficient evidence to assess the benefits versus harms of screening mammograms in this demographic, considering factors such as false positives and radiation exposure.
Navigating Recommendations for Dense Breasts:
For women with dense breasts, who constitute nearly half of those undergoing screening, the guidance remains somewhat ambiguous. While the task force advocates for starting mammogram screenings at age 40 universally, it acknowledges limitations in the effectiveness of mammograms for this demographic. Notably, there is insufficient evidence to endorse supplemental screenings such as ultrasounds or MRIs for women with dense breasts.
Individuals identified as high risk for breast cancer, including those with genetic markers like BRCA1 or BRCA2 variations, fall outside the purview of the new recommendations. Instead, the task force emphasizes the importance of comprehensive assessment and genetic counseling for such individuals, as outlined in previous guidelines.
Understanding Insurance Coverage for Mammogram Screenings:
Despite the revised guidelines, insurance coverage for mammograms is unlikely to change significantly. Most insured women in the U.S. already benefit from coverage for screening mammograms, commencing at age 40 and occurring biennially or annually, based on existing recommendations from medical and scientific bodies. Whether through employer-based insurance, private insurance, or Medicaid expansion programs, the majority of women are entitled to these essential screenings without cost-sharing, ensuring continued access to preventive care.