Source-nhlbi.nih_.gov
Impact of Social Determinants on Sickle Cell Disease Outcomes
A recent study has revealed that preschool-aged children with sickle cell disease (SCD) who reside in food deserts and lack access to transportation face a higher risk of hospitalization and acute complications. Despite receiving free, evidence-based therapy and social support, these children experience significant health disparities, according to findings published in Blood Advances. Senior author Dr. Jason Hodges, director of research at St. Jude’s Children’s Research Hospital, highlighted that while comprehensive care is offered, there remains a gap in addressing community-based challenges such as transportation and food access, which impact the health outcomes of these patients.
The study focuses on community-level social determinants of health (SDoH), which include factors like income level, education, transportation, and proximity to grocery stores. While previous research has shown the effect of SDoH on children with SCD, this study delves deeper into how these specific community factors contribute to the health disparities seen in SCD patients.
Key Findings on Community-Level Factors
The researchers analyzed data from 435 children, aged 0-6 years, enrolled in the Sickle Cell Disease Clinical Research and Intervention Program. Participants’ home addresses were mapped and compared with census data on poverty levels and food access. The results showed that children who lived in households located more than a mile from a grocery store had a 44% higher rate of hospitalizations and a 37% increase in acute care utilization (ACU). Additionally, the absence of a vehicle in the household further increased the risk of hospitalizations.
In contrast, households with an adult holding a bachelor’s degree saw a 33% reduction in ACU and hospitalizations, indicating that parental education may play a protective role in the health outcomes of children with SCD. All participants in the study were Black, with 43% living in neighborhoods identified as particularly vulnerable. Despite receiving standard care such as hydroxyurea and monthly transfusions, disparities persisted, underscoring the importance of addressing external community factors.
Implications for Public Health Policy
Lead author Hamda Khan, a clinical research associate at St. Jude’s, emphasized that without addressing fundamental issues like food access and quality of life in under-resourced neighborhoods, providing holistic care for SCD patients will remain a challenge. Both Khan and Dr. Hodges advocate for public policy changes that target high-need areas, bringing more resources and interventions to improve outcomes for SCD patients. They also suggest that future research should investigate other environmental SDoH, such as air pollution and household size, to gain a better understanding of how these factors affect children with SCD.
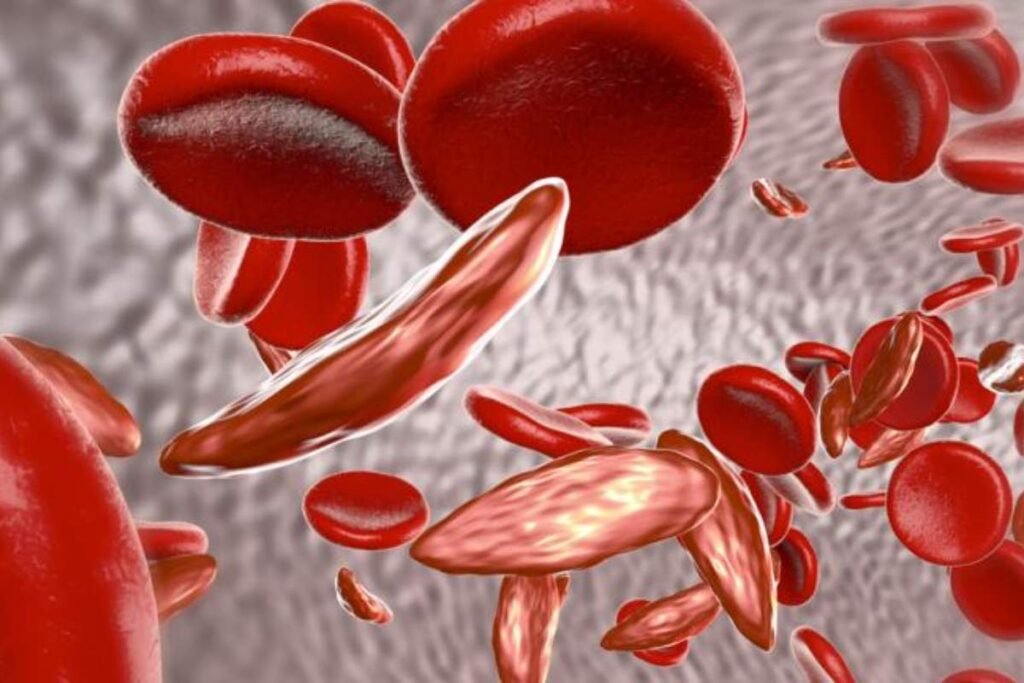
While the study offers valuable insights, the authors caution that the findings are specific to children aged 0-6 receiving comprehensive care and may not apply to older patients or those living in areas with better resources. Sickle cell disease remains the most common inherited blood disorder in the United States, affecting around 100,000 people, predominantly within the Black and African American communities. The study’s results highlight the urgent need for targeted public health initiatives to address the deep-rooted social challenges affecting this vulnerable population.